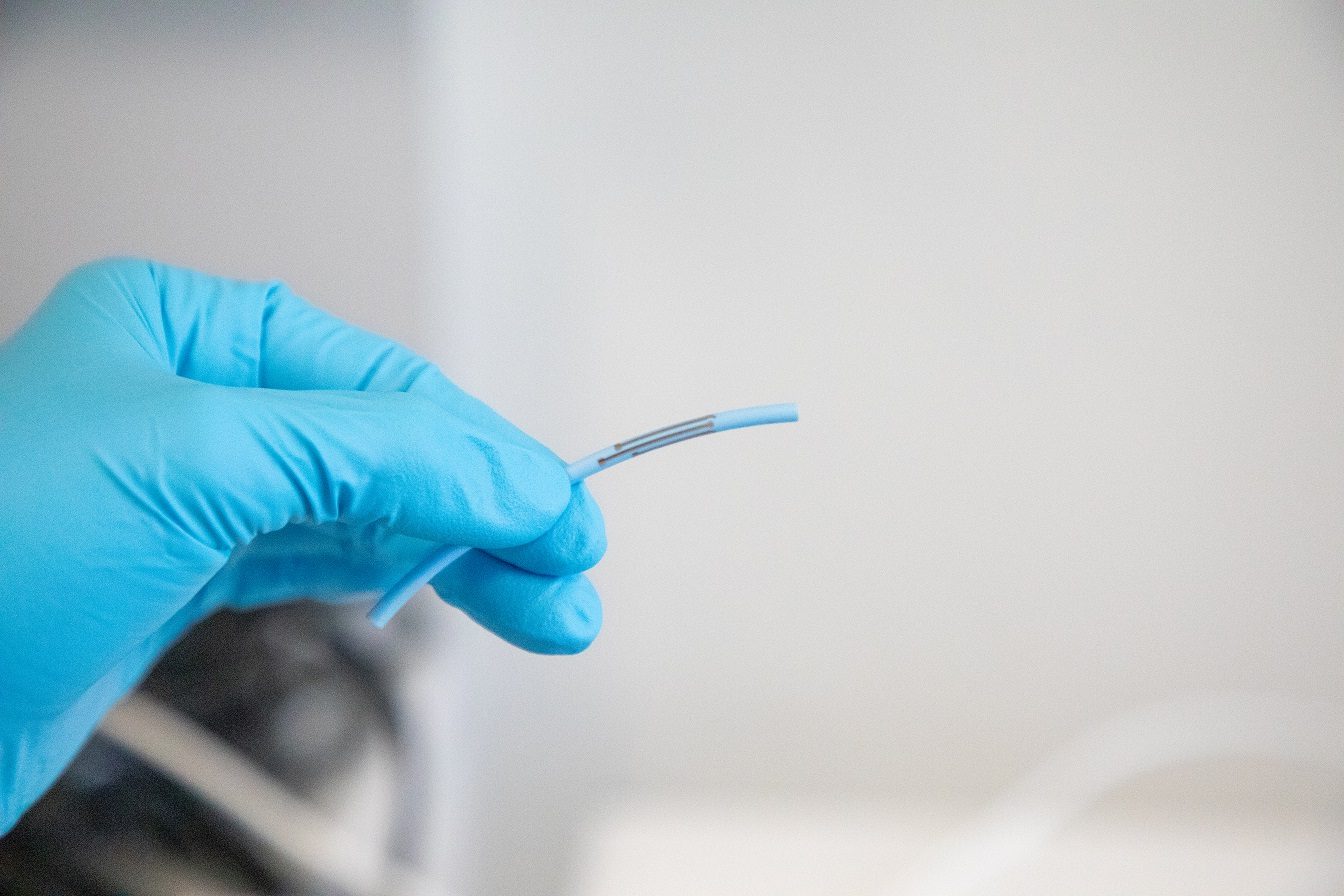
Catheter with enhanced functionalities |
Medical Need
Critically ill patients often present rapid deterioration of vital signs as a consequence of various underlying diseases, making frequent blood tests necessary. While cardiovascular and respiratory monitoring is usually available online at the bedside using standard monitoring systems for hemodynamics and mechanical ventilation, results of laboratory parameters are often delayed at least for some hours. Although point-of-care devices are available at the bedside for certain parameters, e.g. blood gases and some coagulation tests, a considerable amount of blood is used when those tests are applied frequently.
We aim at developing smart sensors, placed on clinically used indwelling catheters to provide real-time in situ monitoring of essential laboratory parameters. This approach will enable individualized therapy guidance, improving quality of care, patient safety and outcome in critically ill patients.
Blood parameter test, central venous catheter, implantable sensor, continuous monitoring
Journal of Clinical Medicine | 2022 Apr 25
Real-Time Monitoring of Blood Parameters in the Intensive Care Unit: State-of-the-Art and Perspectives
D. Karnaushenko, B. Ibarlucea, S. Lee, G. Lin, L. Baraban, S. Pregl, M. Melzer, D. Makarov, W. M. Weber, T. Mikolajick, O.G. Schmidt, G. Cuniberti, Light weight and flexible high performance diagnostic platform, Adv. Healthc. Mater., 4 (10), 1517–1525 (2015).
Spieth PM, Guldner, A, Huhle, R, Beda, A, Bluth, T, Schreiter, D, Ragaller, M, Gottschlich, B, Kiss, T, Jaber, S, Pelosi, P, Koch, T, Gama de Abreu, M. Short-term effects of noisy pressure support ventilation in patients with acute hypoxemic respiratory failure. Critical care. 2013;17(5):R261.
M. Fischer, M.F. Maitz, C. Werner. Coatings for biomaterials to improve hemocompatibility. Hemocompatibility of Biomaterials for Clinical Applications. In Hemocompatibility of Biomaterials for Clinical Applications; Blood-Biomaterials Interactions, 163-190 (2018). Woodhead Publishing – Elsevier, Sawston (UK).
Project team members |
High-tech |
Abstract |
Even if point-of-care devices and rapid processing central laboratory services are available, these measurements remain discontinuous and do not enable individualized treatment approaches in dynamic and rapidly changing critical situations. Furthermore, a considerable amount of blood is needed when laboratory tests are applied frequently, sometimes even requiring transfusion of blood or blood products. Real time measurement of key parameters (e.g. lactate, electrolytes, glucose, oxygenation, acid-base status) would improve patient care and individualized treatment. Indwelling catheters are routinely placed in critically ill patients to allow hemodynamic monitoring and/or administration of potent drugs. We aim at developing smart electrochemical micro-sensors, placed on such indwelling catheters to provide continuous monitoring of essential parameters, without increased consumption of blood or use of additional sensor interfaces. Such sensors will integrate all necessary components on a smart catheter for reagentless and real time analysis, including selective membranes that protect the surface from deterioration. Therefore, online measurements of key laboratory values such as blood gases would certainly improve quality of care towards more individualized therapeutic approaches. Moreover, the measurement of glucose and lactate levels would allow direct monitoring and response in dynamic situations in critically ill patients. Glucose plays a central role when monitoring liver function in patients with multi-organ failure or acute diabetic states e.g. after total pancreatectomy. Lactate is one of the best established markers representing adequate tissue (micro-) perfusion, frequently used in different states of shock, especially for guiding fluid resuscitation and differentiated catecholaminergic support. This approach will enable patient-centered, individualized therapy guidance and therefore improve quality of care, patient safety and outcome in critically ill patients.

