AI-generated synthetic data for cancer research and clinical trials
AI-based solutions for cost-effective cancer treatment decisions
Published in the Cell Press journal Trends in Cancer, the article addresses the growing complexity of treatment options for solid tumors and the socio-economic disparities in accessing personalized medicine. The researchers highlight the potential of cost-effective biomarkers – derived from routine medical imaging and electronic health records – to support the selection of cancer therapies and reduce the workload of healthcare professionals.
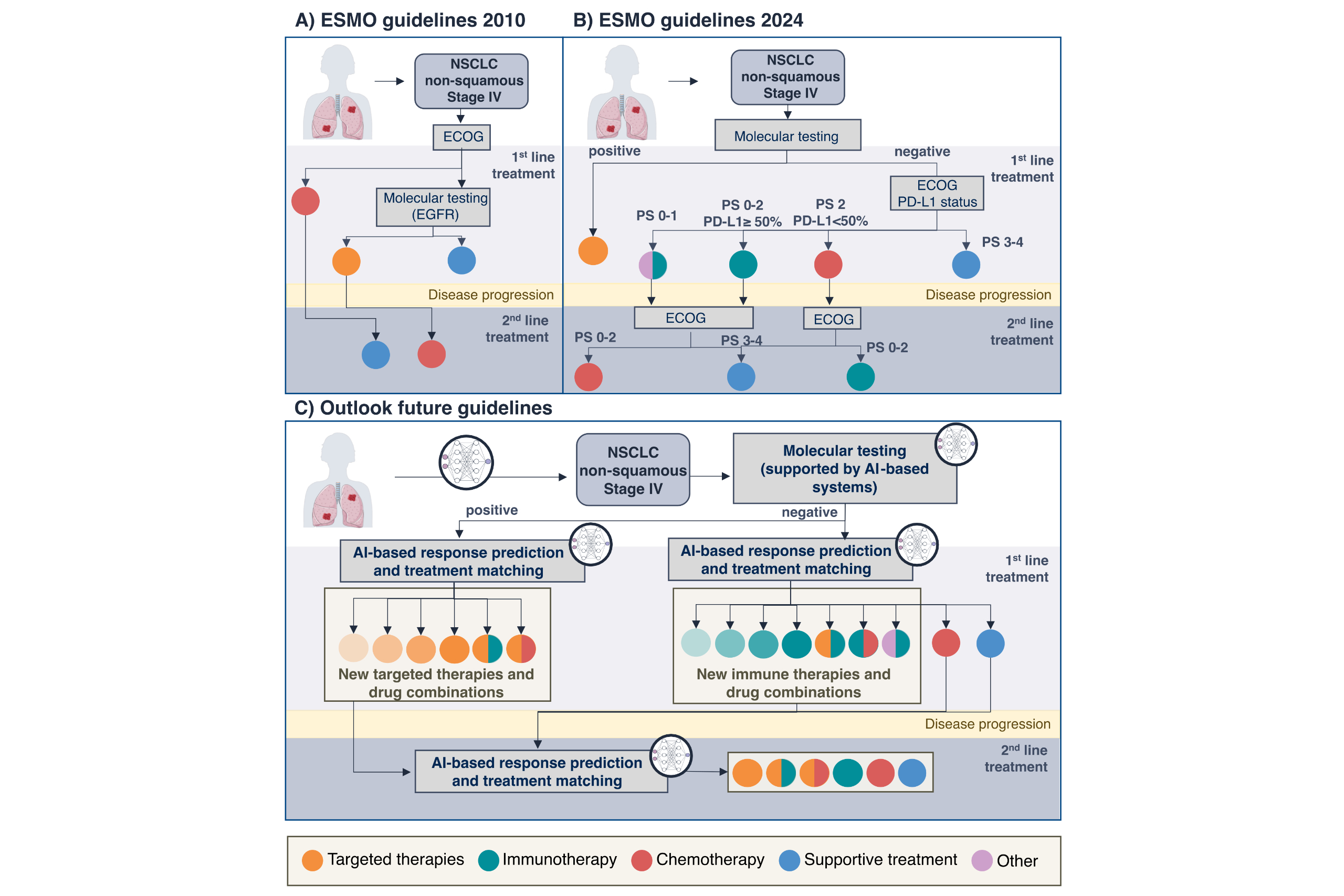
Treatment landscape for solid tumors has become increasingly complex, making it challenging for physicians to identify the optimal therapy for each patient. In addition, the high costs associated with personalized medicine testing often limit their widespread accessibility. AI-based biomarkers present a promising solution to these limitations.
“AI methods – such as deep learning and large language models – can help identify biomarkers from routine medical data such as pathology images, radiology scans, and clinical reports to find patients most likely to respond to specific therapies. The application of AI-based biomarkers offers a cost-effective approach to support treatment decisions and access to personalized medicine,” says Dr. Marta Ligero, lead author of the publication and scientist in Professor Kather’s research team at EKFZ for Digital Health in Dresden.
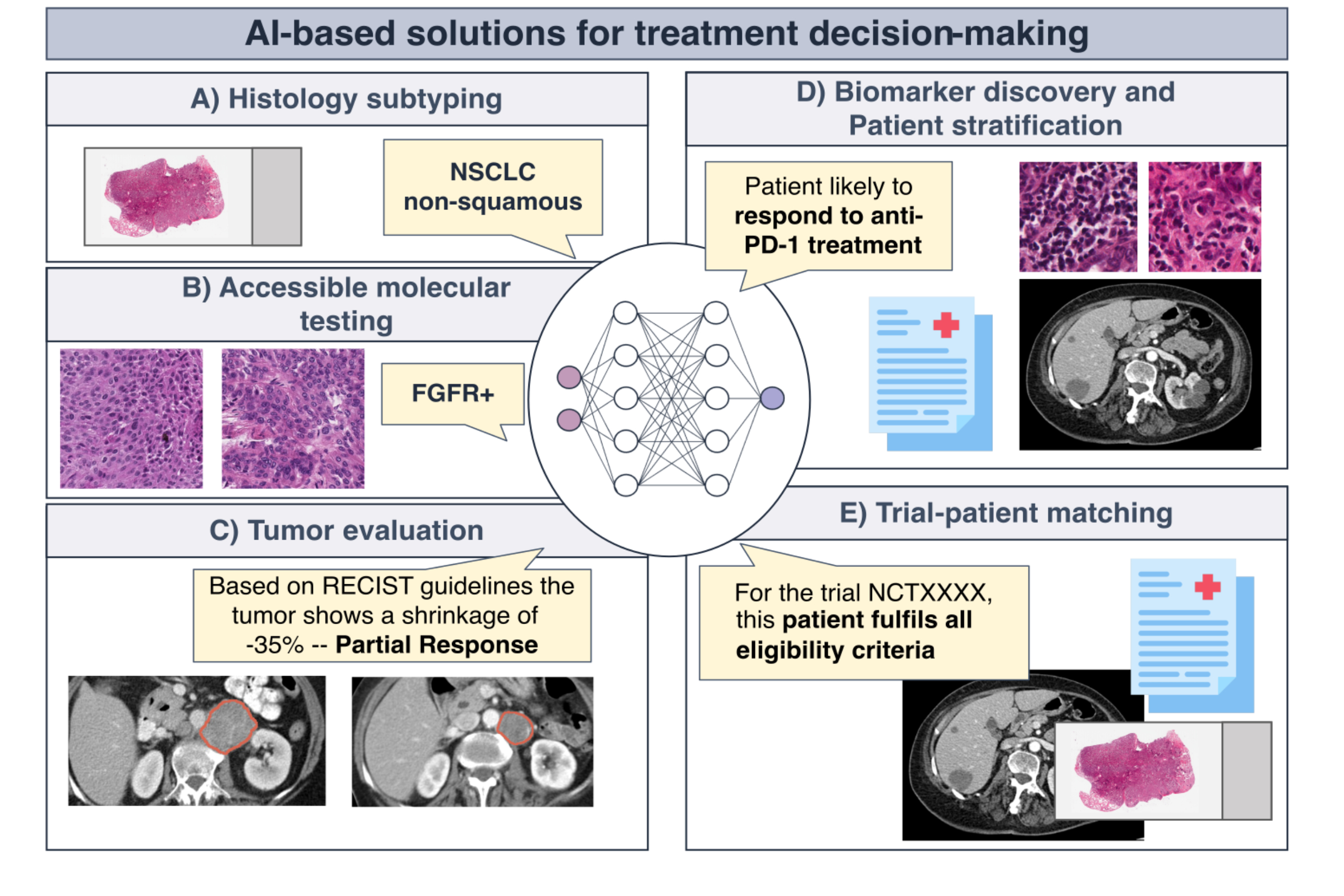
Improved cancer treatment decisions by AI-based applications
There are several ways, how AI models can enhance cancer treatment. They can help automate clinical tasks that currently require manual input from physicians, such as classifying histopathological cancer subtypes directly from medical images. This automatization could enable faster treatment decisions while reducing the workload of healthcare professionals. Another relevant application is the prediction of molecular biomarkers from routine medical imaging. This approach can overcome the limitations of next-generation sequencing, which currently involves high costs, specialized expertise and long turnaround times, making personalized therapies more accessible. Additionally, AI-based tools can streamline patient-trial matching, easing the workload of multidisciplinary teams and improving patient eligibility evaluations. Finally, by identifying novel patterns in clinical data, AI solutions can discover new clinical and molecular properties that could determine if a patient is suitable for a specific therapy.
Current limitations and next steps towards routine clinical implementation
Despite their potential, AI-based methods face several challenges that need to be addressed before widespread clinical adoption. Most importantly, AI-based biomarkers need to be carefully evaluated through large-scale studies and prospective trials. In addition, the authors emphasize the need for clear regulatory guidelines to accommodate the development and approval of AI-based solutions. Economic feasibility studies and algorithmic fairness are necessary to ensure equitable implementation of AI-based biomarkers.
“AI-based biomarkers will constitute a significant proportion of all biomarkers in precision oncology within the next decade. As treatment decision trees grow increasingly complex, the need for additional biomarkers continue to increase. However, their safe integration into clinical practice requires appropriate legal and regulatory frameworks,” explains Prof. Dr. med. Jakob N. Kather, Professor of Clinical Artificial Intelligence at TU Dresden and oncologist at Dresden University Hospital Carl Gustav Carus. “In addition, it will be important for medical practitioners and researchers to develop AI literacy – a basic understanding of AI methods – to be able to effectively evaluate and apply these biomarkers as they become more widely available,” he adds.
More News
Carl Gustav Carus Awards for three EKFZ affiliated young researchers






