
Holistic digitalization of a minimal invasive and high precise autotransplantion therapy for the treatment of cleft and lip palate |
Medical Need
Cleft lips and palates are the most frequent facial malformations. Their treatment is interdisciplinary in many steps over several years. Depending on frontal tooth eruption during the child’s development bone grafting for repair of the cleft alveolus is required. Although in own and other studies, grafting of tissue engineered bone is promising, autologous bone from the hip is the gold standard. Several tools (osteotomes, trephine drills, chisels) are used, however, the harvesting process and the grafting procedure are not clearly determined in respect of mechanical loads influencing bone cell vitality and fitting of the graft into the bone defect, leading to gaps between graft and recipient site. These are crucial points to warrant an optimal grafting volume and a good healing without complications at the donor and the recipient site. This is particularly rewarding as cleft surgery is mainly done in children.
The project aims to improve the healing process and the outcome of bone grafting in cleft patients by supporting the surgeon with data driven decision taking methods. We want to demonstrate how to adjust the processes and tools – supplying the systems used with sensors and smart controls – to make them accessible for methods as they are used in modern cutting edge industrial technology (Industry 4.0).
Cleft Surgery, Bone grafting, Sensors, Digitalization
Journal of Personalized Medicine | Volume 12 | Issue 3, 2022: A Holistic Approach for the Identification of Success Factors in Secondary Cleft Osteoplasty
W. Pradel and G. Lauer, “Tissue-engineered bone grafts for osteoplasty in patients with cleft alveolus,” Ann. Anat. – Anat. Anzeiger, vol. 194, Nov. 2012.
P. Korn et al., “3D Printing of Bone Grafts for Cleft Alveolar Osteoplasty – In vivo Evaluation in a Preclinical Model,” Front. Bioeng. Biotechnol., vol. 8, Mar. 2020.
A. Ben Achour et al., “The Influence of Thrust Force on the Vitality of Bone Chips Harvested for Autologous Augmentation during Dental Implantation,” Materials (Basel)., vol. 12, Nov. 2019.

Project team members |
High-tech |
TU Dresden, Faculty of Mechanical Science and Engineering
Institute of Mechatronic Engineering, Chair of Machine Tools and Adaptive Controls and
Fraunhofer Institute for Machine Tools and Forming Technology,
Department of cyber-physical production systems
Fraunhofer Institute for Machine Tools and Forming Technology,
Department of cyber-physical production systems
Abstract |
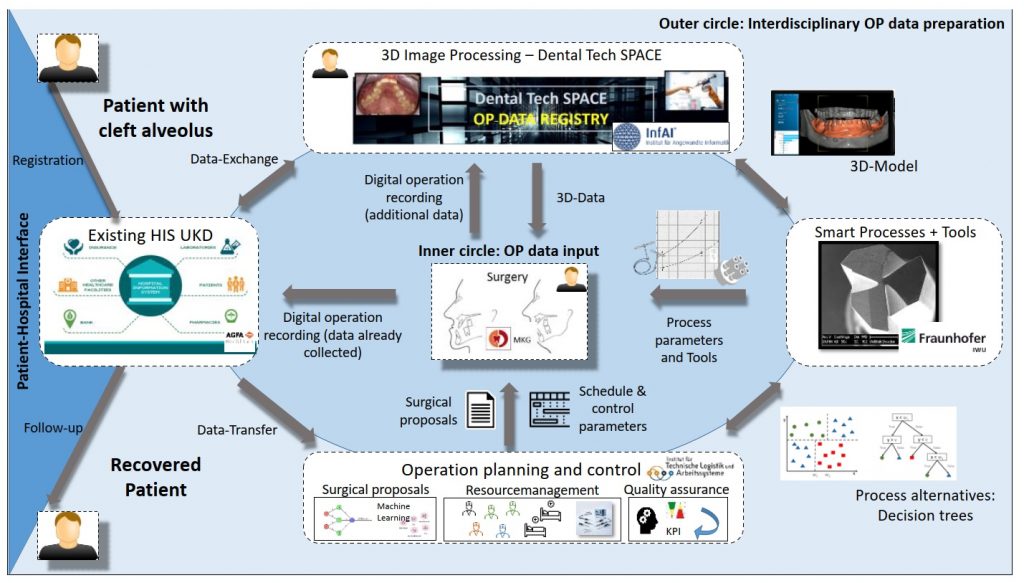
Cleft lips and palates are the most frequent facial malformations. Their treatment is interdisciplinary in many steps over several years. At a certain point in the child’s development bone grafting for repair of the cleft alveolus (Figure 2) is required. Autologous bone from the hip is the gold standard. Several tools (osteotomes, trephine drills, chisels) are used, however, the harvesting process and the grafting (carving) procedure are not clearly determined in respect of mechanical loads influencing bone cell vitality and the fitting of the graft into the bone defect. The interdisciplinary project team is developing a routine with digital methods for a standardization and optimization of bone grafting surgery for complexly-shaped bone defects using the cleft alveolus as example in a lab scale. Using 3D models generated from medical images special physical training models are produced. Mechanical loads during bone graft harvesting, carving and fitting are recorded with sensors in combination with 3D navigation. The accuracy of the grafts is checked on the physical model and the influence of the individual process steps on the cell vitality and important growth factors is being investigated. These data are managed and exchanged with existing hospital information systems by an enhanced dental tech space. Based on the clinical situation, a planning and control strategy is developed. For this purpose, machine learning is used in order to enable optimal timing in the planning and control phase of the surgery. In the vision, the holistic digitalized therapy should be integrated into a clinical set-up (Figure 1). Finally, this knowledge will be also transferable into the treatment of other bone defects.

